One of the critical aspects of this pandemic is having meaningful and granular data that can be used to make decisions. We are very thankful to the COVID-19 Immunisation Task Force (CITF) and the Ministry of Health (MOH) for the data made available on ‘github.com’. It has been useful to help understand the pandemic and many bright Malaysians have given us some good analysis from that data set.
However meaningful data has three characteristics: they must be transparent, granular and timely (or “in real-time”). We understand the struggles to post real-time data and we have improved somewhat with data transparency. But we still have no access to granular data. Without granular data we are unable to understand the needs down to the district/state level, cannot get a profile of risk, have difficulty monitoring the outbreak regionally, and may not be able to respond to local health service needs.
Granular data is required to answer the many questions the public have, such as: Is testing adequate in my district or state? Are the health services coping well in my district or state? Which hospitals need our help the most? Who is most likely to get severe illness? What is the risk of severe illness to young adults and children with the Delta variant? How effective is vaccination at preventing severe illness? And many other questions.
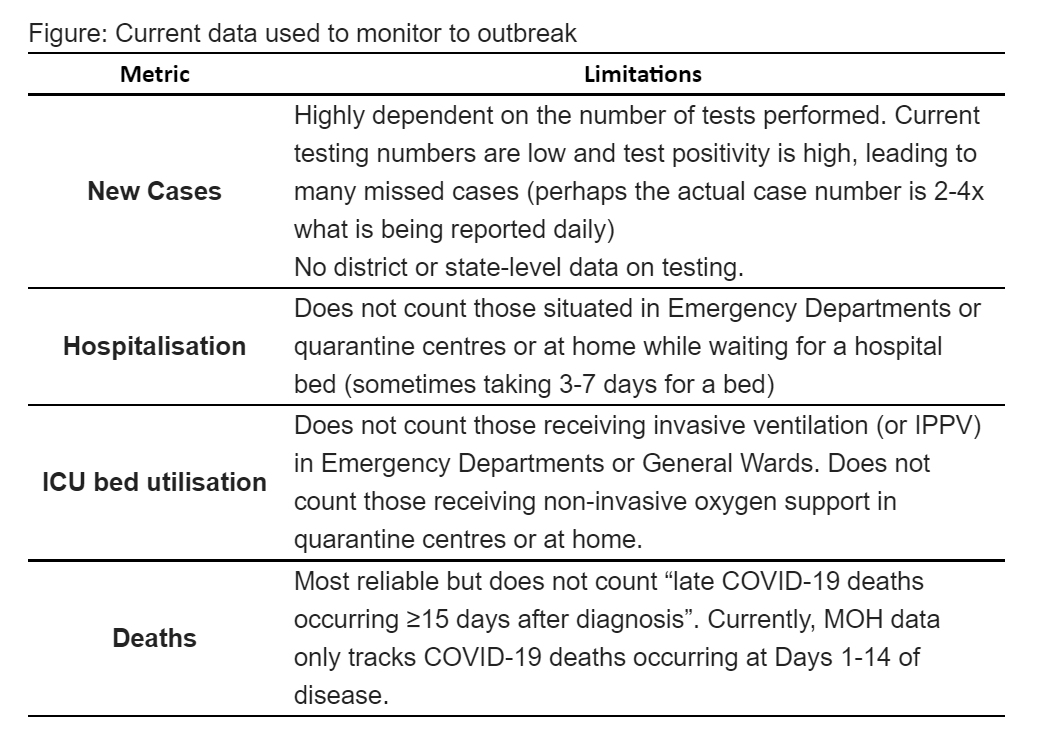
Limitations of Current Data (Metrics) used to Monitor Outbreak
The figure below summarises the issues with the data that is currently used and shared with the public.
1. Daily Case Numbers
Daily case numbers are what the public looks at and are often used to describe worsening or improvement. But case numbers are entirely dependent on testing numbers. No data on testing numbers by district or state is made available so we have no idea of what case numbers mean by district or state. The national test positivity rate has remained high (10-15% for the past three weeks) indicating that the overall testing numbers are far too low and we are missing many who are positive.
2. Hospitalisation Number
This could be a better indicator to tell us what is happening but it becomes of little value once hospital beds are fully occupied. Then those that are managed in the Emergency Departments or waiting to get admitted from the quarantine centres are not counted. So it can give a false idea of the situation.
3. ICU Bed Utilisation
The use of ICU beds should be one of the best metrics to monitor the situation but it becomes meaningless once the ICU beds are fully occupied. Those on ventilation in the general wards and Emergency Departments are currently not counted, and neither are those on NIV (non-invasive ventilation) waiting in quarantine centres or at home. So we are not given a clear picture of the situation. For example, in the Klang Valley, for every person in an ICU bed there are possibly 2-3 who need an ICU bed but cannot get it. This also applies to many states outside of the Klang valley like Kedah, Perak and Sabah.
4. Deaths
Death numbers are the most reliable data but it is delayed data and is a lagging indicator (2-3 weeks from infection). Additionally, late COVID-19 deaths are not counted (died ≥15 days after diagnosis). In addition, we hope all unexplained deaths at home are tested for COVID-19.
Useful Parameters to Monitor
Outlined below are some useful parameters to monitor the outbreak. Our health staff are overloaded and we need to bring in manpower from other ministries to help collect and upload these data.
1. Severity of Illness by Location Daily
A useful data set to monitor would be the category of illness for those COVID-19 positive (Category 1 to 5) and deaths (including brought in dead) by location and by district/state.
This means having data on where the Category 1 to 5 patients (and deaths) are located (i.e., which facility, either in an ICU, general ward, Emergency Department, quarantine centre or at home). This is required by state and district. If we see all our Category 4 to 5 patients are in an ICU and all our deaths occur in hospital, then we know the health service is able to cope. If we see most of our Category 4-5 patients are dying at home, then we know the health service has lost control. This data will also inform civil society which region is decompensated and require support.
2. Highest Severity of Illness
Ideally we require the highest category of illness (Category 1-5 and Death) after COVID-19 infection by all granular variables – location (facility), age, sex, ethnicity, comorbidity, state, district and stratified by detailed vaccination status (no vaccination, 1 dose, 2 does, 14 days after 2nd dose, type of vaccine). This data will enable us to answer many questions on vaccine efficacy, risk for severe illness and death, and other relevant questions.
3. Detailed Testing Numbers
Providing testing numbers by district and state would help make sense of daily case numbers and show the adequacy of testing. Even more valuable would be to show data on contact tracing. Specifically, we must answer these questions: of those confirmed positive, how many contacts were identified, how many contacts tested positive, and how fast contact tracing was done from positive confirmation to final contact informed.
4. Vaccination Data by Granular Variables
While we have general data on vaccination we lack details – age, sex, ethnicity, comorbidity by locality. This granular data is vital as we try to reach every adult in our community. It offers a profile of who has accepted vaccination and helps to identify those who need vaccination. Elected representatives and others can then work to target groups that are vaccine hesitant or missed to boost our vaccine uptake.
5. Collateral Deaths
It would be important to monitor collateral morbidity and mortality for other non-COVID-19 conditions; i.e. those who had some other illnesses and had a worse outcome as they could not get appropriate care. This will offer data to allow rebalancing of our health service.
In summary, choosing the most meaningful and appropriate indicator to monitor our pandemic will allow for a better grasp of its severity, where additional resources are required and when regions can have further relaxation of SOPs. When services are overrun, COVID-19 clinical category and deaths by facility daily is an important metric to add to our data transparency efforts.
This opinion piece was contributed by Dato’ Dr Amar-Singh HSS and Dr Khor Swee Kheng. If you have an article or opinion that you would like to contribute for the benefit everyone, share it with us here.
[ IMAGE SOURCE ]








