This post is brought to you by Subang Jaya Medical Centre.
Our hearts beat to keep us and every organ in the human body alive and well, just like how a tiny motherboard is responsible for powering up our devices. This is why it’s important that we keep our hearts in tip-top condition and beating strong.
So for folks who aren’t aware, there is a proper rhythm to our heartbeat and this is how doctors know our hearts are fine. When our heart beats with an irregular rhythm, there is a risk of what is known as Arrhythmia.

To find out more, we sat down with Dr Koh Kok Wei, a cardiologist specialising in the electrophysiology of the heart at Subang Jaya Medical Centre (SJMC).
Right, so what is arrhythmia?

A healthy human heart beats 60 times a minute at rest with a constant rhythm. This is regulated by the heart’s intrinsic pacemaker or natural pacemaker called the sinus node. It’s a small collection of specialised cells located at the top of the right atrium that produce the electrical impulses that cause the heart to beat.
When the sinus node generates an electrical impulse, the current travels down across the atria causing it to contract. This is the lub sound you hear. It then pauses at the atrioventricular (AV) node which sits between the atria and ventricle before being relayed across the ventricle, causing it to contract. This makes the dub sound.
However, when the sinus node is damaged or other atrial tissues generate rogue electrical impulses, the heart will develop an abnormal heart rate known as arrhythmia. There are 3 parent categories of arrhythmia which are abnormally slow heartbeat, fast heartbeat, and irregular heartbeat.
A slow heartbeat is called bradycardia, a fast heart rate is called tachycardia, and an example of an irregular heart rate is atrial fibrillation (AFib). While the effects of the other two are self-explanatory, AFib is a little more complicated. As the name implies, it occurs in the atria which is the upper chamber of the heart, specifically the right atrium.
The action of the right atrium fibrillating can be described as shivering, causing the atria muscles to partially contract up to 600 times per minute. This leads to the chaotic and irregular beating of the atria which causes it to be out of sync with the ventricle or lower chamber.
Gotcha! But what causes arrhythmia?

Arrhythmia is the product of other heart-related diseases, and a common example would be a heart attack. In some cases, the condition could have developed congenitally or hereditary. But often, the cause of arrhythmia is just part of the ageing process.
As we start to age, the heart’s tissues start to degrade and die as it can’t regenerate healthy cells. So, when intrinsic heart tissue cells start to degenerate, that’s when arrhythmia may occur. Individuals over the age of 65 have a higher risk of developing AFib, though it can occur in much younger individuals.

But before ageing can cause arrhythmia, the failure to maintain a healthy heart can lead to it first. Hypertension or high blood pressure makes the heart pump harder to push the blood through.
The same can be said about valve regurgitation or in layman’s terms, leaky valve. It’s a condition where one of the heart’s valves doesn’t close properly, allowing blood to flow backwards through the valve instead of moving forward. So, the heart needs to work harder to circulate the right amount of blood through the body.
This causes the heart to work overtime and over a prolonged period, it can cause the heart to enlarge, strain out, undergo fibrosis and develop arrhythmia.
When blood is cut off to the heart during a heart attack, parts of the heart muscle start dying off. When heart tissue dies, it cannot recover as the cells are unable to regenerate. Normally, that would cause scarring of the heart tissues, leading to a weakened heart.
In short, any heart issues can increase the risk of developing arrhythmia, even myocarditis which is inflammation caused by an infection.
Born with errors in the electrical system

Sometimes, the natural process produces a heart with errors in the electrical system. Some have congenital arrhythmia which means they are born with the condition and is not necessarily hereditary. Many medical practitioners believe that these individuals have additional electrical accessory pathways which leads to tachycardia.
An individual may not experience any sort of high heart rate at a younger age because the electrical system in the heart develops over time. But they will start manifesting the symptoms upon reaching a certain age.
The additional pathways channel the electricity coming into the ventricle, back to the atria. From there, they will connect to the main pathway and go through it, activating the ventricle again before the next programmed beat. As a result of this action, the heart rate can increase to as high as 200 bpm and in rare cases, can lead to sudden cardiac death.
Hereditary heart disorders can also be a culprit. If there’s a family history of sudden death at a young age with no identifiable cause, then that genetic mutation could be present in you. A genetic test can be conducted to evaluate the risks.
There’s still a lot about the human body that remains unexplained. One of these is why some cases of arrhythmia are idiopathic, meaning it arises spontaneously with no identifiable risk, aetiology, or sickness. You could be an athlete with a tailored diet and ample exercise for a healthy heart, and yet develop arrhythmia for which the cause is unknown.
So how will arrhythmia affect my health?
Each type of arrhythmia has a different effect on your health. When someone develops tachycardia, they will experience palpitation which is a pounding heart from the elevated heart rate. Then there’s giddiness leading to fainting from tachycardia and bradycardia.
This can be dangerous to anyone in any given situation, however, it’s especially more dangerous for the elderly who are more fragile. However, fainting is the best-case scenario as tachycardia and bradycardia can lead to cardiac arrest.
AFib meanwhile takes a different approach. An irregular beat every two regular beats can take a toll on the heart. So imagine the kind of damage a 300 bpm fibrillation can do. The heart undergoes fibrosis where the atrial tissues die and enlarge.
However, that’s not the only way that AFib can affect your well-being. When blood is not being pumped out of the atrium effectively, excess blood pools in the atrial chamber which is not immediately dangerous.
The danger arises when blood starts to pool in a small pouch that protrudes from the top of the left atrium called the left atrial appendage. Blood here becomes stagnant and starts to coagulate forming a blood clot.
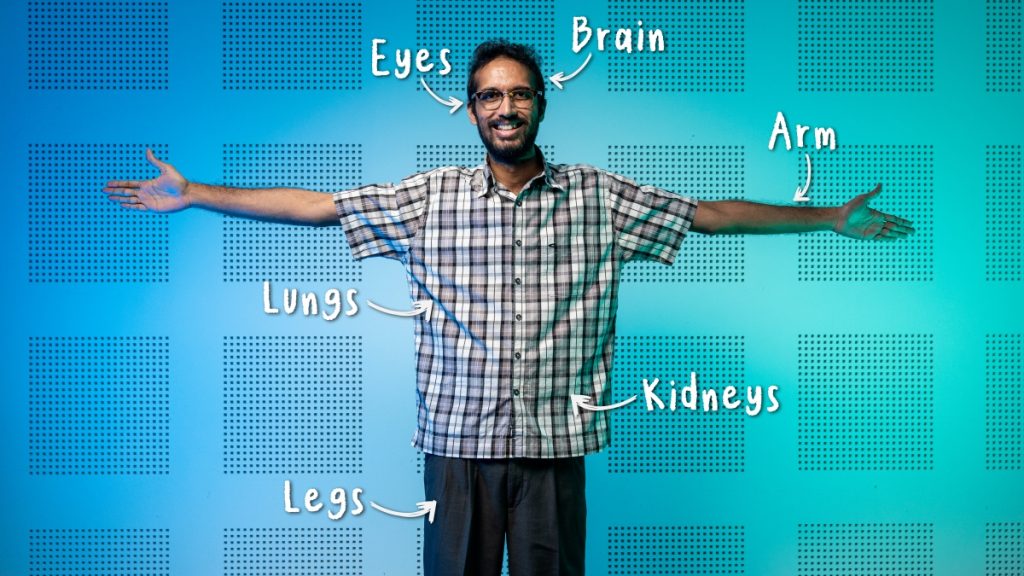
In an unfortunate circumstance, the clot can dislodge and flow up to the brain where it gets stuck and causes a stroke. Or it could flow down and get stuck in the leg causing gangrene which needs amputation. It can even get stuck in the kidney or gut as well.
How do I know if I have arrhythmia?

Most young people who experience tiredness or anxiety will chalk it up to stress-related factors. However, these symptoms could be due to arrhythmia. Coincidentally, the first diagnosis of AFib is not detected by using an electrocardiogram (ECG), but through physical examination of the pulse when an individual comes in complaining about the symptoms.
Tachycardia and bradycardia are easy to identify thanks to obvious symptoms like palpitation and fainting respectively. AFib can cause these symptoms as well, but only in extreme cases. Moreover, a mild case of AFib is an intermittent occurrence and therefore has a lower chance of being detected during a medical checkup.
So the best way to identify AFib is to check your pulse regularly. This way, you will know when something is off with your heartbeat.

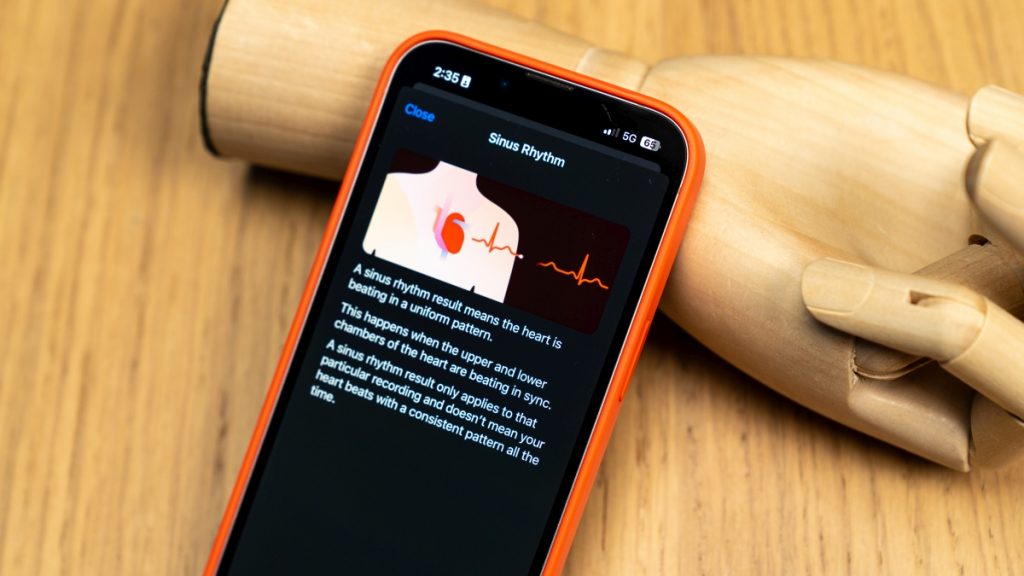
Alternatively, you can take an ECG test to check the electrical activity of the heart for signs of AFib. Thanks to the advancements made in medical tech, there’s no need to go to a hospital. You can run an ECG test using medical-grade ECG devices which reads your heart’s electrical activity and sends the data to a companion app on your smartphone.

Speaking about smartphones, there are medically approved consumer smartwatches in the market that are equipped with an ECG reader. One advantage these smartwatches have is that they can do passive monitoring by using machine learning to predict the possibility of AFib based on the nature of the heartbeats.

In any case, neither a smartwatch nor a medical-grade ECG device can provide a diagnosis, so you’ll need to show the results to a medical practitioner.
What are my options to fight against arrhythmia?
The goal of an electrophysiologist is to try and correct or compensate for the rogue electrical impulses generated by defective cells. In general, each type of arrhythmia is treated differently, but based on the situation, the treatments can be shared.
Bradycardia – Slow Heart Rate
To remedy this, a pacemaker is implanted to regulate the heartbeat by generating an artificial electrical impulse. This causes the heart to beat faster thus circulating blood through the body at the correct rate.
Tachycardia – Fast Heart Rate
A pacemaker can generate electrical impulses, but it cannot stop excessive electrical impulses. Therefore, the cells responsible for the unwanted electrical impulses must be stopped.
To do so, radiofrequency ablation (RFA) is used to ablate or destroy part of the dysfunctional electrical conduction system of the heart. Ablation catheters are inserted at the groin through a small puncture hole and channelled to the heart.
That said, some cases of tachycardia can be treated through oral medication that will reduce the heart rate.
AFib – Irregular Heart Rate
RFA can be used to treat AFib with good outcomes, however, it is unable to guarantee the recurrence in the future as the individual ages. Therefore, the individual needs to be constantly protected from a stroke caused by a blood clot. So, an oral anticoagulant is prescribed to thin the blood and reduce the chance of blood clot formation.
That being said, a medical practitioner can implement a combination of a pacemaker, RFA, or medication to treat the arrhythmia.
Can you explain more about the pacemaker?
A pacemaker is an implantable medical device that generates artificial electrical impulses to regulate the heart rate. Some units come with remote system monitoring that can wirelessly transmit data recorded for the day to an online server which can be accessed by a medical practitioner for review.
Generally, the device is used to treat bradycardia but can be used to treat other arrhythmias if needed. There are two categories of pacemakers which are conventional pacemakers and the newer leadless pacemakers.
Leaded Pacemakers
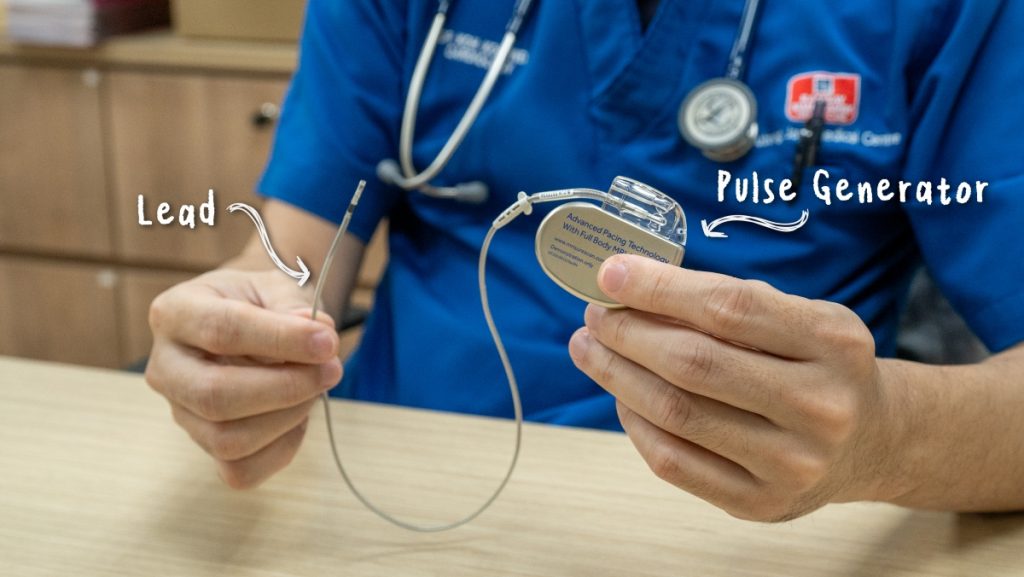
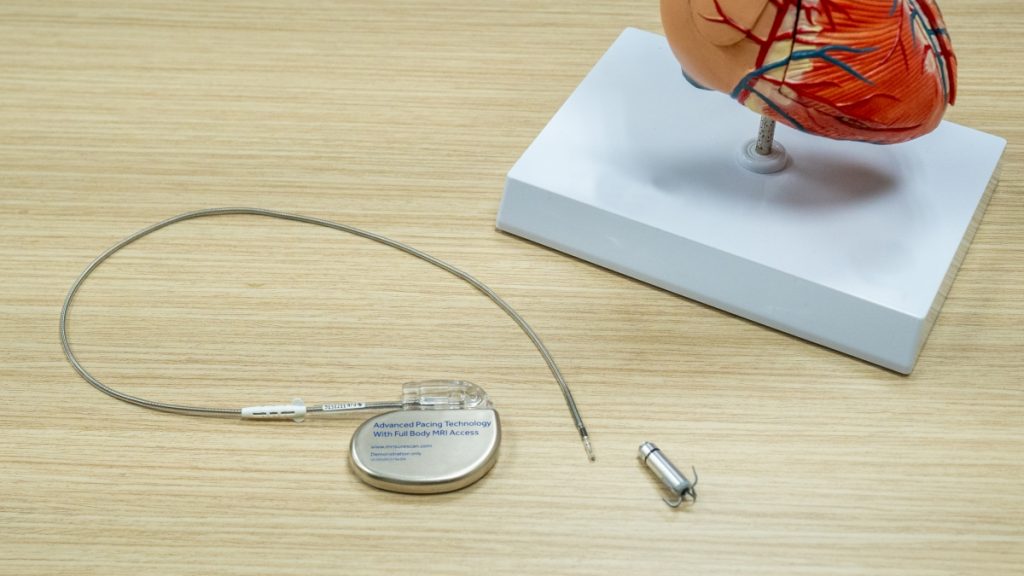
The conventional pacemaker has been helping individuals with arrhythmia for the last 40 years. It is composed of two components: the pulse generator and leads. The pulse generator is the visibly larger component that houses the battery and electronic circuitry that is used to create an electrical impulse.
Meanwhile, the leads connect the pulse generator to the heart and house the electrodes and sensors. Depending on the situation, a conventional pacemaker can have either one or two leads. These are referred to as a single-chamber system pacemaker and a dual-chamber system pacemaker, respectively. Often, it is the dual-chamber system pacemaker that’s implemented to synchronise both the atria and ventricles.
The leads are channelled into the heart chambers through veins with the first option being the subclavian vein near the left collarbone as it leads directly to the heart. As for the pulse generator, it sits outside of the heart, nestled under the subcutaneous tissue, which is the deepest layer of the skin.
Based on the situation, the pulse generator will only kick in when the heart rate drops below the programmed threshold. For example, when the heart rate drops below 50 bpm, the pacemaker will start pacing the heart by generating electrical impulses to increase the heart rate. Once the heart can maintain a healthy rate, the pacemaker goes into standby mode and continues to monitor the situation.
But this raises a good question – what if you’re exercising and the minimum heart rate to maintain is now higher? Does the pacemaker still look for the 50-bpm minimum threshold? To solve this, a pacemaker is fitted with sensors to detect physical movement and increase the minimum heart rate threshold accordingly.
As for battery life, it’s rated for up to 10 to 13 years and minor surgery is required to swap the dead pulse generator unit with a new one. Additionally, the leads may start fracturing after compressing and stretching to the movement of the heart and body for a long period, usually after 20 to 30 years. Extracting the fractured lead is difficult because the vein tissues have scared over the leads, essentially enclosing it.
So they are just left alone and new leads are inserted into the vein and channelled to the heart. Over time, the vein gets clogged up and new leads cannot be inserted. This isn’t a concern for the elderly, but it is a concern for the youth. In this case, the medical practitioner will consider other veins leading to the heart.
However, using other veins may not be a viable solution always. Individuals on dialysis or undergoing chemotherapy require the use of veins as well. Moreover, the vein is delicate, so it gets blocked off or closes off when meddled with. This prevents a pacemaker from using the same vein later.
Besides challenges with the leads, the pulse generator has its own set of requirements. For one, the skin needs to be thick and strong enough to hold the pulse generator. Additionally, the skin tissue needs to be healthy. If there’s an infection after the pulse generator has been implanted, it will be immediately removed, and the individual placed on antibiotics for a minimum of six weeks.
During this period, they will need an alternative solution to regulate the heart rate. Besides these issues, there will be visible a scar left over from the operation to implant the pacemaker.
Leadless Pacemaker
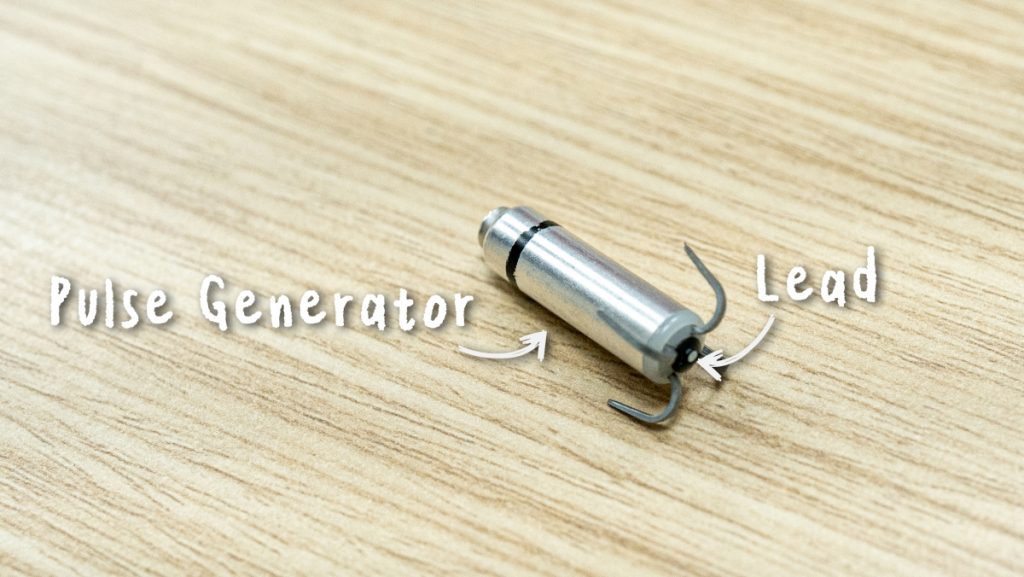
Leadless pacemaker is a relatively new invention and is not a replacement for conventional pacemaker as we will find out later. Unlike a conventional pacemaker, a leadless pacemaker is just a single unit making it the world’s smallest pacemaker. The pulse generator, sensors, batteries, and circuitry are contained in a cylindrical housing while the electrode is located at the bottom of the housing, surrounded by claws.
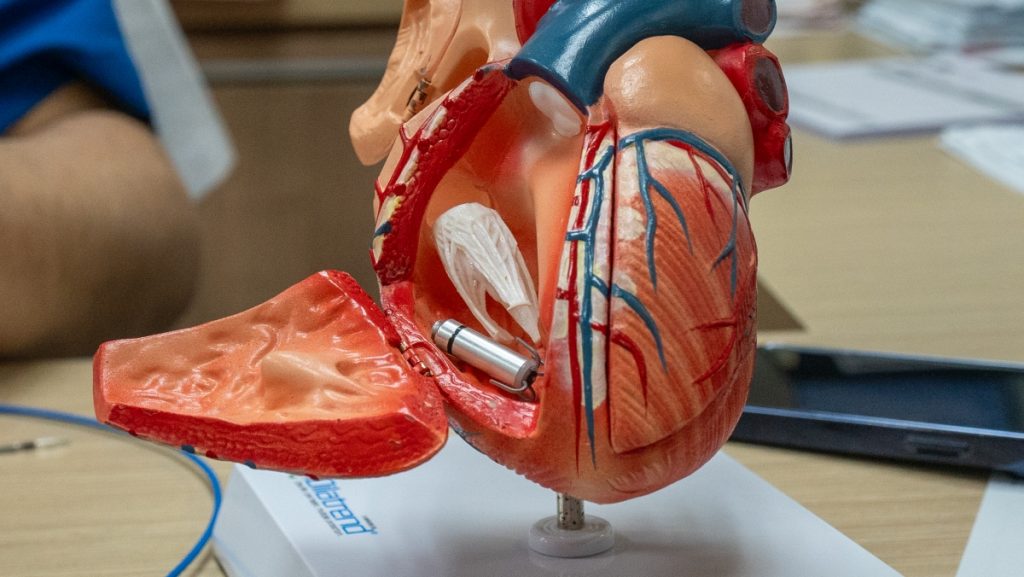
Since the electrode is integrated into the housing, the whole unit needs to be implanted in the heart. On the other hand, the device doesn’t depend on the veins to function. A 1 cm incision is made at the groin and the leadless pacemaker is directed to the right side of the heart through the femoral vein and implanted in the ventricle. Seeing how the incision at the groin is small, the scarring is minimal with the worst-case scenario being a slight crease.
Without the need for a vein to function, it is a great alternative option for those undergoing dialysis or chemotherapy, and the lack of a bulky pulse generator means it’s also best for frail individuals with thin skin.
However, there’s a reason why the ventricle was specifically mentioned during the implantation process. That’s because the leadless pacemaker is a single-chamber system pacemaker which only paces the ventricle. In conditions like AFib where the right atrium is just fibrillating making it difficult to pace, a leadless pacemaker can be deployed to just pace the ventricles.
There are versions of the leadless pacemaker with sensors that can detect when the atria have contracted and sync the ventricles accordingly. However, it still can’t physically pace the atria, and in conditions with irregular heartbeat, the unpredictable nature makes it difficult to sync.
So in general, a leadless pacemaker is not suitable for situations where both the atria and ventricles require pacing. Here, a conventional pacemaker is still required.
In terms of lifespan, the batteries in the leadless pacemaker are rated for 10 years of use. When the leadless pacemaker is no longer functional, a new unit is implanted in the ventricle. The non-functional unit can be surgically removed, however, that’s a challenging feat given that heart tissue has scarred over it.
The million-dollar question: Can arrhythmia be cured?
To answer the question that’s on all of our minds – can arrhythmia be cured? We will need to look at the type of arrhythmia we’re dealing with. Treating certain arrhythmias like supraventricular tachycardia with radiofrequency ablation therapy has more than a 95% chance of successfully restoring normal heart rhythm.
Remedying AFib early may produce good outcomes. That said, since the risk of developing AFib increases with age, there’s a possibility it will rear its ugly head again. Therefore, you will need to continue monitoring your heart.
Unfortunately, if you need a pacemaker for bradycardia or other similar conditions, then that is for life.
If it’s for life, do I need to make any lifestyle changes?

Should you have to live with a pacemaker, there are little to no lifestyle changes you need to make. For the first two months, limit movement of the shoulders as there’s a 3% to 5% chance that the tiny screws keeping the lead attached to the heart chamber might dislodge if tugged on too hard. Other than that, just be sure to keep the wound clean and infection-free.

The pacemaker can be disrupted by strong electromagnetic interference (EMI) like the ones emitted by an electrical generator at a power plant. So unless you work next to one, you shouldn’t be too concerned. Many consumer electronics don’t emit high EMI, but it’s always recommended that you read the warning labels on electronic devices before using them near a pacemaker.
Besides EMI, electrical leakage can confuse a pacemaker. For example, if your electric shower or electric water heater isn’t grounded correctly, there will be an electric current in the water touching your body. This current causes the sensor on the pacemaker to detect a false reading that indicates the heart rate is high when in fact it is dropping. As a result, you can faint in the shower. If this happens, be sure to check if the wiring is done correctly.

Other than that, you can continue the lifestyle that you were living before receiving a pacemaker.
There’s very little to worry about the pacemaker surgery
Dr Koh Kok Wei has been implanting pacemakers for more than a decade now and he assures that there is nothing to worry about when undergoing a pacemaker surgery as the procedure is generally safe. As a matter of fact, it is safer than other cardiac-related procedures.
Drop by Subang Jaya Medical Centre and speak with Dr Koh Kok Wei

Subang Jaya Medical Centre (SJMC) is an award-winning hospital with an impeccable reputation that spans nearly 4 decades for medical excellence in healthcare. The hospital has many senior doctors with rich experience and pioneers in the medical field like Dr Koh Kok Wei who have vastly improved the lives of patients who come through our doors.

When SJMC first opened in 1985, it was the first private hospital to perform open heart surgery in Malaysia. Since then, it has been a pioneer in adopting the latest advancements in medical technology like the world’s smallest pacemaker, the leadless pacemaker.
Get in touch with SJMC today and have your heart examined.








