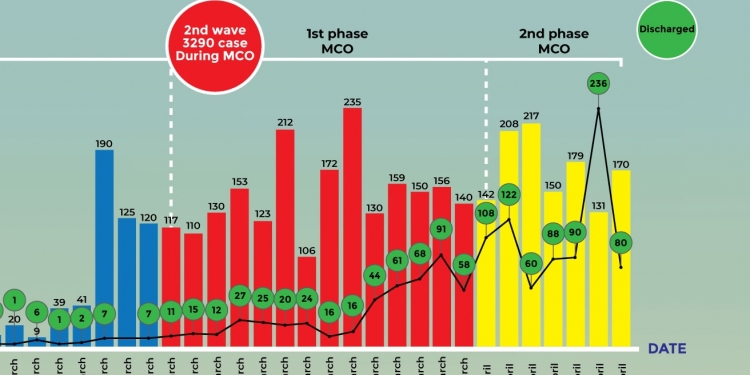
There are many individuals who have expressed reassurance with the small number of daily new coronavirus cases reported and the slow growth of our epidemic. I have seen many posts on various social media regarding this, often with some comparison with countries doing worse than us. But this is false reassurance if you look at the bigger picture.
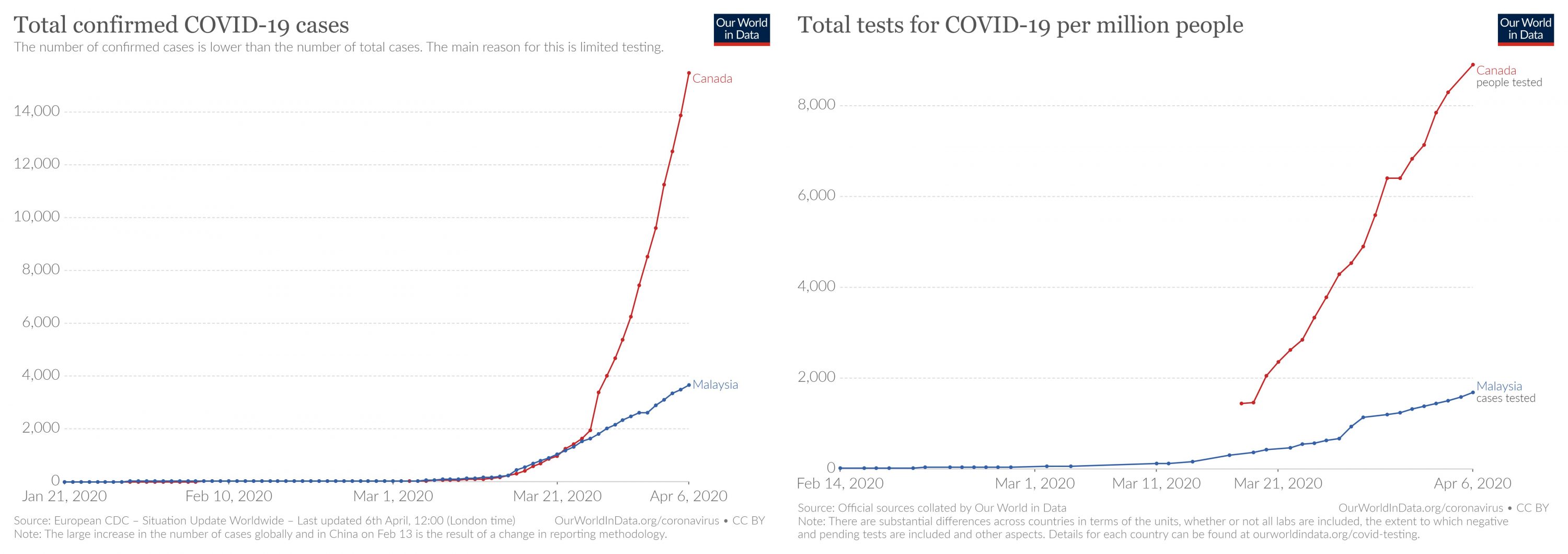
The number of tests we do determines the cases we find and report. If we compare Canada and Malaysia, a comparison I have seen online as our population sizes are similar, you will note (on the left) that they have many more cases than us. But also note (on the right) that they do a huge number of tests per million population compared to us. The stark similarity of both graphs speaks for itself. In this epidemic, you get the numbers you test for.
Allow me to illustrate how we could look at the data regarding our epidemic. I am trying to answer the question: “What is the size of the coronavirus epidemic in Malaysia?”
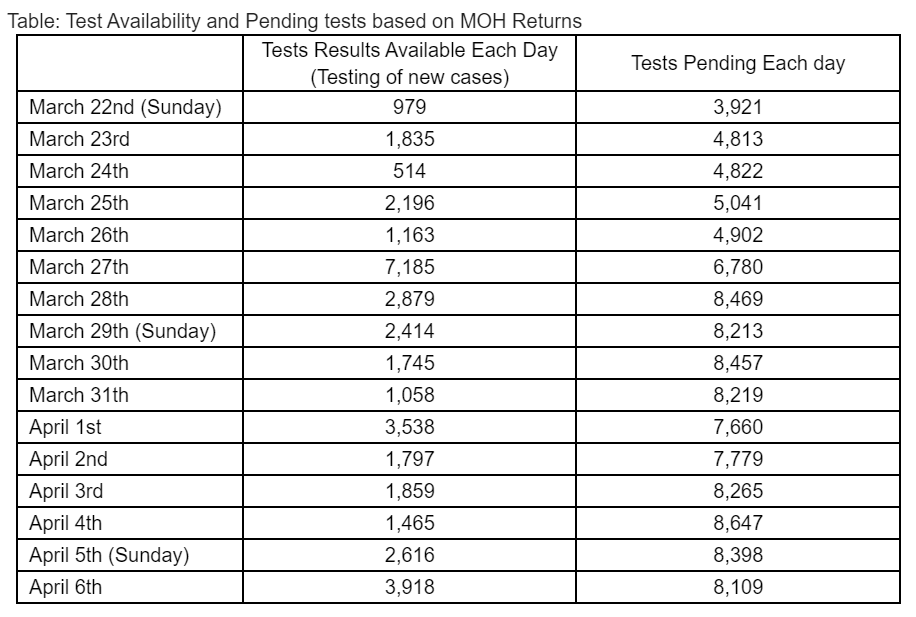
First, recognise that our testing numbers are limited. MOH only does what they call ‘targeted’ testing and does not test widely outside of that criteria. The table below shows the test results available each day from the testing of new cases for the past two weeks. Except for one outstanding day (27th March), our test availability are generally between 1,500-3,500 each day. We have been informed by the Ministry of Health (MOH) that currently, we can do 11,500 tests each day. However, only about 20% of these tests are used to look for the spread of the virus in the community. The remainder are used to re-test confirmed cases with a view to determine discharge ability, treatment response and possibly repeated tests for suspected cases that are negative the first time [polymerase chain reaction (PCR) tests depends on quality of the sample and have only 60-70% positivity for nasal swabs or sputum].
Secondly remember that our testing capacity is limited by many challenges. The large number of pending results each day indicates we are having difficulties with getting tests done. Imagine for a moment that we could clear these tests and get all the results. 5-10% would come back positive (using MOH daily positivity rates) and that would mean additional 400-800 cases – possibly a 20% jump in total numbers.
You may have read how, four days ago, that Sabah obtained 5,000 test kits from Singapore as they did not have reagents to do the PCR tests. The Sabah authorities commented that the reagent test kits received would last only one week and that they had a backlog of 3,000 samples to process.
MOH had informed that the PCR test (identifies the virus genetic material) takes 6-7 hours to conduct and that results are usually available within 24 hours. Although we would like to get our test results back within 24 hours, this is not always possible. A number of colleagues working on the ground have expressed that getting results in 48 hours is considered a good response. Some say it takes 5-7 days to get results. Even health care staff that have potentially been exposed may have to wait for 4-5 days to get their status known.
All this indicates problems with testing ability, supply of reagents and turnaround time. Despite 34 laboratories in action (private laboratories and hospitals have been recruited to support testing and currently more than 20 are able to do so) we still have more work to do to clear our backlog of tests and improve test turnaround time.
Thirdly remember that because we do ‘targeted’ testing, we may miss coronavirus infections in other settings. Allow me to give some common examples of what is happening all over the country.
A 70-year-old man comes to one of our hospitals. He had a fever and respiratory symptoms for a few days. He now has a bad pneumonia and needs oxygen and intubation (ventilation support). He has no known contact with a COVID-19 patient or history of travel but there is a real possibility that he might be infected with the coronavirus. Imagine the risk to all the health care professionals managing him and the family/community he lives in if we do not test him? Until the past two days, MOH local guidelines did not advocate testing any such patients.
From MOH Influenza-Like Illness (ILI) & Severe Acute Respiratory Infection (SARI) surveillance that is conducted at selected sites, about 1.2% of these patients have been COVID-19 positive in the past week. This indicates community spread, as these persons have no contact with known cases. We do not know how many patients with pneumonia and severe respiratory illnesses (influenza-like illness) we have missed in the past 4-6 weeks.
We have also not been testing unlinked pneumonia deaths routinely and may have underestimated the real number of COVID-19 deaths in the country. Our Statistics Department (2018 data) notes that pneumonia deaths are the second commonest cause of death in Malaysia and account for 11.8% of deaths. This amounts to 390 pneumonia deaths per week. Even if only 1.2% of these pneumonia deaths were due to COVID-19 (from surveillance data) it still accounts for an extra 30-40 coronavirus deaths in the past 2 months. Note that the presence of another virus identified in these patients does not exclude co-infection with COVID-19, as it has been shown in other countries.
Another area we are limited in testing is our health care professionals (HCPs). While we will test those exposed to COVID-19 positive patients, we do not routinely test HCPs who become unwell with respiratory symptoms. In this epidemic the highest risk job is that of a HCP. Every day they will see countless patients, some who may be infected with the coronavirus without their knowledge. We may assume that the greatest risk is to HCPs working in ICU with the severely ill COVID-19 positive patients, but that may not be true. These staff usually have adequate personal protective equipment (PPE). The ones most at risk are those working in casualty, out-patients department, GP clinics and any general ward or clinic. It is well established that children and young adults may look quite well but be infected (30-50% asymptomatic infections). It is in these locations that PPE is currently inadequate. Many staff have had to rely on homemade (not all reliable) or donated PPE. We are still struggling with the distribution of national PPE supplies. Even as far back as 20th March, MOH reported that 15 HCPs had been infected by COVID-19 as part of their work.
Finally, the data reported each day shows the growing number of cases not linked (unlinked) to any cluster (at least 20-30%). Even the known clusters have not had full testing of all known contacts. We are also aware of a growing concern of outbreaks in tahfiz school communities.
Hence the daily numbers of positive tests reported daily are a poor indicator of the size of our epidemic in Malaysia.
We return to our original question on “What is the size of the coronavirus epidemic in Malaysia?”
We could rely on researchers and scientists internationally who do modelling and try to understand the numbers that are missed (not identified by the health system). They suggest that we should at least double or triple the number identified. Some models suggest multiplying our reports by a factor of ten. Our reported numbers yesterday were 3,793. If we include pending tests and use a factor of three times, then possibly we have 13-14,000 cases.
Another way to estimate the size of our epidemic is to use deaths; what is called a ‘back-of-the-envelope calculation’. If we assume a reasonable (good) mortality rate of 1% (no one is sure of the actual mortality rate as yet). Then 1 death = approximately 100 cases. We currently have 62 deaths which equates to 6,200 cases. But remember that deaths have a lag-time compared to cases. It takes about 7-14 days before an infected person presents clinically. It takes another 7-14 days before illness severity and dying (ventilation and ICU care). Hence about 3-4 weeks ago we possibly had 6,000 plus cases in our country. What is it like today? Remember we will have missed deaths by our restricted testing policy and that, from international data (especially NHS, UK), half of those in ICU on ventilation may sadly die.
Hence the correct answer is “We don’t know how big our epidemic is” but it is definitely bigger than reported numbers. Our limited testing number and criteria do not allow us to have a clear grasp of the spread of the virus.
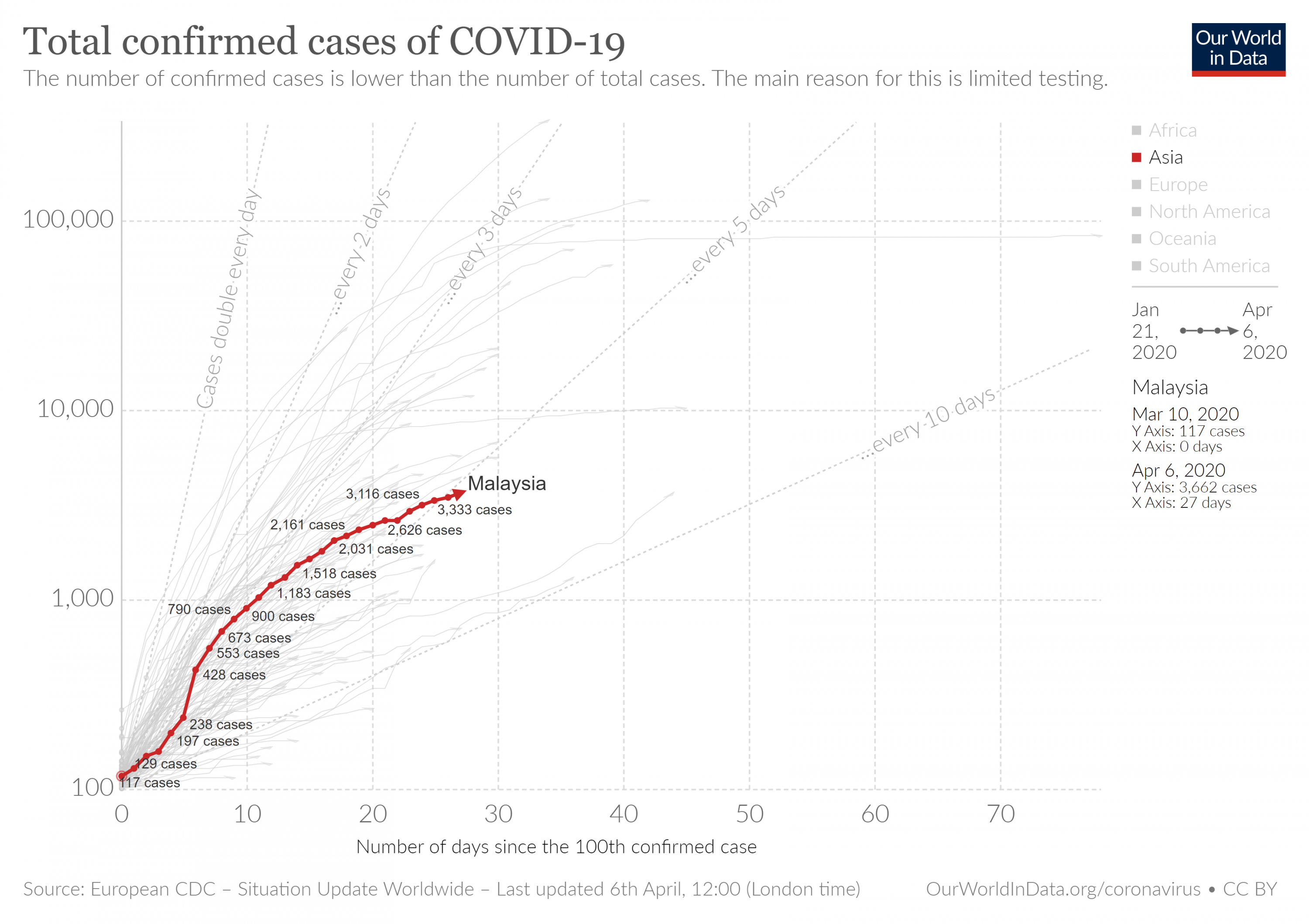
The graph from ‘Our World in Data’ shows that we are not the worst country but neither are we the best country. We must benchmark ourselves with countries with progressive health systems like South Korea, Taiwan and Singapore that have made a difference in this pandemic.
The World Health Organisation has emphasized the need to test adequately to identify infected individuals and reduce secondary infections. It has stressed the need to prevent infections among healthcare workers and not allow any transmission amplification events. The Movement control order (MCO) has been vital in curbing the coronavirus epidemic in our country but we cannot keep the MCO indefinitely. It is hurting our poorer Malaysians severely. Our public need good/correct information and accurate and extensive data. This will allow everyone to make an informed decision and act in the best way.
This epidemic will show us how we as people are able to face major challenges. It will reveal how good our health services are and if we had adequately invested in them. It will test the quality of our leadership in the difficult days ahead.
This opinion piece was contributed by Dato’ Dr Amar-Singh HSS, Senior Consultant Paediatrician. If you have an article or opinion that you would like to contribute for the benefit everyone, share it with us here.
[ IMAGE SOURCE ]